Can My Baby Have Pedialyte? Your Go-To Guide for Safe Hydration During Illness
Let’s face it, few things are as heart-wrenchwrenching as seeing your little one under the weather. A fever, a tummy bug, or just a general lack of sparkle can send any parent into a spiral of worry. And when your baby isn’t eating or drinking well, the biggest concern often becomes dehydration. You might find yourself wondering, "Is Pedialyte the answer? Can my baby drink Pedialyte safely, or is it just for older kids?"
It’s a totally valid question, and one that countless parents ponder. In those moments of uncertainty, you want clear, compassionate, and actionable advice, not just medical jargon. You’re looking for reassurance and practical steps to help your precious bundle feel better. That’s exactly what we’re here for!
This comprehensive guide will walk you through everything you need to know about Pedialyte and babies. We’ll explore when it might be helpful, what signs to look for, and most importantly, why always checking in with your pediatrician is your number one priority. By the end, you’ll feel more confident and empowered to navigate these challenging times, armed with knowledge to support your little one’s well-being.
Can Babies Drink Pedialyte? What Parents Need to Know
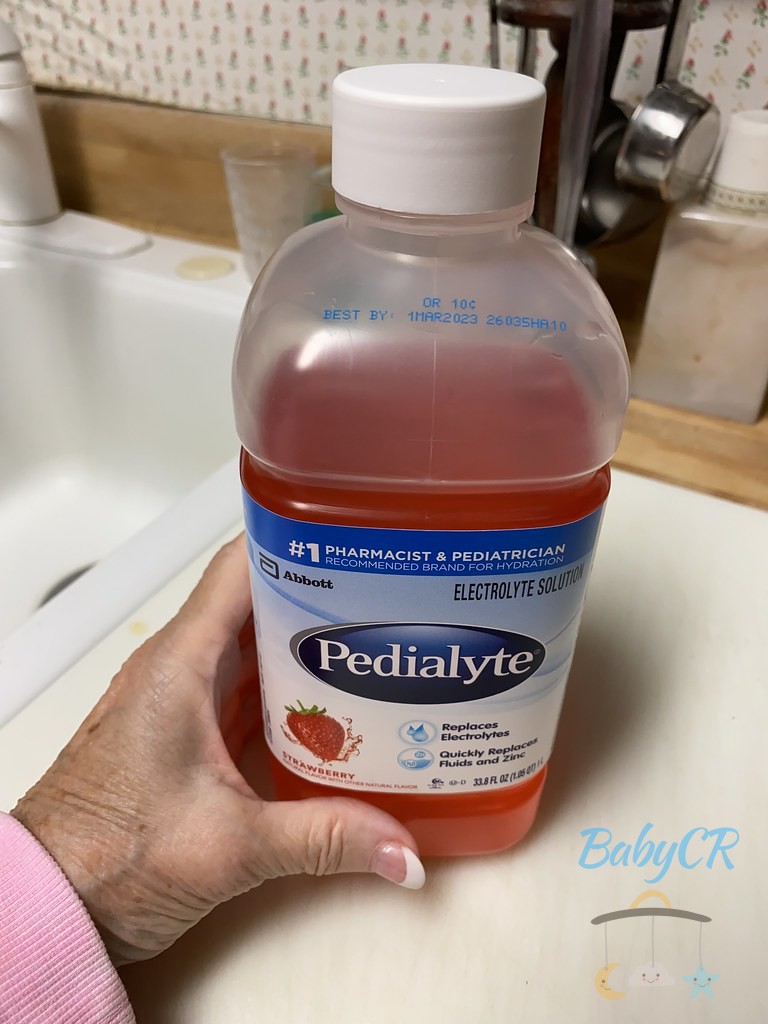
When your baby isn’t feeling their best, especially with vomiting or diarrhea, fluid loss can happen surprisingly quickly. This is where the thought of an oral rehydration solution like Pedialyte often pops into a parent’s mind. It’s a common over-the-counter product designed to help replenish fluids and electrolytes, which are crucial minerals that help the body function properly.
The short answer is yes, babies can drink Pedialyte, but it’s not a one-size-fits-all solution and comes with very important caveats. It’s specifically formulated to provide a balanced mix of water, salts, and sugars that the body needs to absorb fluids effectively when it’s experiencing significant losses. Unlike plain water or juice, Pedialyte aims to restore the delicate balance of electrolytes without overwhelming a compromised system.
However, it’s absolutely crucial to understand that Pedialyte should never be given to a baby without prior consultation with a pediatrician, especially for infants under six months of age. Your baby’s doctor is the best person to assess their specific needs, determine if Pedialyte is appropriate, and provide precise instructions on dosage and duration. Their little bodies are incredibly delicate and require tailored care.
Understanding Pedialyte: More Than Just Water
You might be thinking, "Why can’t I just give my baby water or watered-down juice?" That’s a great question, and it highlights why Pedialyte is uniquely formulated for certain situations. Pedialyte isn’t just flavored water; it’s an oral rehydration solution (ORS) meticulously designed to mimic the body’s natural fluid balance.
When a baby experiences fluid loss due to illness, they don’t just lose water; they also lose essential electrolytes like sodium, potassium, and chloride. Plain water can’t replace these vital minerals, and in some cases, giving too much plain water to an infant can even dilute their existing electrolytes, leading to serious complications. Similarly, juice often contains too much sugar and not enough electrolytes, which can actually worsen diarrhea.
Pedialyte strikes a delicate balance, providing the right concentrations of these electrolytes along with a small amount of sugar. This sugar helps the body absorb the salts and water more efficiently, making it highly effective at rehydrating a dehydrated baby. Think of it as a specialized, rapid-response drink for a body that’s lost its equilibrium.
Age Matters: When Is It Safe?
The age of your baby is perhaps the most critical factor when considering Pedialyte. The younger the baby, the more cautious you need to be, and the more vital it is to consult your pediatrician. Their tiny systems are still developing and are far more sensitive to imbalances than an older child’s or an adult’s.
For infants under three months of age, any significant fluid loss or signs of illness warrant an immediate call to the doctor. In many cases, breast milk or formula remains the primary source of hydration, even during illness, and your doctor will guide you on how to continue these feedings or if an alternative is needed. Introducing anything new, especially an electrolyte solution, without medical guidance could have unintended consequences.
For babies between three and twelve months, Pedialyte might be recommended by your pediatrician if they are experiencing mild to moderate dehydration due to vomiting or diarrhea. However, the type of Pedialyte (some have more sugar than others), the amount, and the frequency will all be very specific. Never assume the dosage for an older child or adult applies to your infant; their needs are entirely different.
Dosage and Administration: Getting It Right
Once your pediatrician has given the green light for Pedialyte, following their exact instructions on dosage and administration is paramount. This isn’t a situation where "more is better" or where you can eyeball the amounts. Too much or too little can be ineffective or even harmful to your baby’s delicate system.
Typically, your doctor will provide a specific amount to offer based on your baby’s weight and the severity of their dehydration. They might suggest giving small, frequent sips rather than large quantities all at once, especially if your baby is vomiting. For example, they might advise offering 1-2 teaspoons every few minutes, gradually increasing the amount as tolerated. This slow approach helps prevent the stomach from getting overwhelmed and triggering more vomiting.
Remember to use a clean spoon, syringe, or bottle to administer the Pedialyte. Never mix Pedialyte with breast milk, formula, or other liquids unless specifically instructed by your doctor, as this can alter its carefully balanced electrolyte composition. Once opened, Pedialyte should be refrigerated and used within 48 hours, as directed on the packaging, to maintain its effectiveness and prevent bacterial growth.
Pedialyte vs. Other Fluids: Why the Specificity?
It’s natural to wonder why Pedialyte is often recommended over other seemingly benign fluids like water, diluted juice, or even sports drinks when a baby is sick. The answer lies in the precise science behind rehydration and the unique needs of a baby’s body. These other fluids, while fine for healthy children in moderation, can actually exacerbate problems during illness.
Plain water, as mentioned, lacks the crucial electrolytes that are lost during vomiting or diarrhea. Giving large amounts of plain water to a dehydrated baby can lead to a dangerous condition called hyponatremia, where sodium levels in the blood become too low. This can cause swelling in the brain and lead to seizures or even coma. Babies, especially infants, are particularly susceptible to this.
Juice, even diluted, is generally too high in sugar and too low in electrolytes. The high sugar content can pull more water into the intestines, potentially worsening diarrhea and leading to further fluid loss. Sports drinks, while containing electrolytes, often have even higher sugar content and artificial ingredients that are not suitable for infants and young children. Pedialyte is specifically designed with the optimal balance for gentle, effective rehydration.
Potential Pitfalls and What to Avoid
While Pedialyte can be a lifesaver in specific situations, there are definite pitfalls to avoid. The biggest one is self-diagnosing and self-treating. Giving Pedialyte without a doctor’s recommendation can mask serious underlying conditions or delay essential medical care. It’s a tool, not a universal remedy for all baby ailments.
Another common mistake is using the wrong type of Pedialyte or administering it incorrectly. There are different formulations (e.g., unflavored, flavored, with probiotics). Always ensure you’re using the appropriate one for infants and following the pediatrician’s exact instructions. Over-administering or giving it too quickly can lead to more vomiting, while under-administering might not provide adequate rehydration.
Finally, remember that Pedialyte is for rehydration, not nutrition. It’s not a substitute for breast milk or formula, which provide vital nutrients for growth and development. Once your baby is rehydrated and tolerating fluids, your pediatrician will likely advise a gradual return to their regular feedings. Prolonged use of Pedialyte in place of their usual diet can lead to nutritional deficiencies.
Knowing When Your Baby Needs Pedialyte: Key Signs
Recognizing the signs of dehydration in a baby can be tricky because their symptoms can sometimes be subtle. However, being vigilant and knowing what to look for is one of the most powerful things you can do as a parent. When a baby loses fluids faster than they can take them in, their body starts to struggle, and prompt action can make all the difference.
Dehydration in infants is particularly concerning because their body weight is composed of a higher percentage of water than adults, and they have a higher metabolic rate, meaning they use and lose fluids more quickly. Their immature kidneys are also less efficient at conserving water. Therefore, what might seem like mild symptoms in an adult can quickly escalate into a more serious situation for a baby.
The key is to observe your baby’s behavior, their wet diaper count, and their physical signs very carefully, especially if they’ve been ill with vomiting, diarrhea, or a high fever. Don’t hesitate to reach out to your pediatrician if you have any concerns at all, no matter how small they might seem. Your parental instincts are incredibly valuable here.
Spotting Dehydration: Early Warning Signals
Being able to identify the early warning signs of dehydration is crucial for getting your baby the help they need promptly. It’s not always as obvious as a baby looking "thirsty" – babies aren’t great at articulating their internal states, so you need to be a detective!
One of the most reliable indicators of hydration status in infants is their wet diaper count. A healthy baby should have at least 6-8 wet diapers in a 24-hour period. If you notice significantly fewer wet diapers, or if their diapers are much lighter than usual, this is a major red flag. Other signs include a dry mouth and tongue, a lack of tears when crying (especially for babies older than 2-3 months), and sunken eyes. You might also notice that the soft spot (fontanelle) on top of their head appears sunken.
Beyond these physical signs, pay attention to your baby’s behavior. A dehydrated baby might seem unusually sleepy or lethargic, less playful, or irritable and difficult to console. They might have cool, clammy skin, or their hands and feet might feel cold even if the rest of their body is warm. Any combination of these symptoms, particularly when coupled with illness, warrants immediate medical consultation.
Common Scenarios: When Dehydration Strikes
While dehydration can occur for various reasons, there are a few common scenarios where babies are particularly vulnerable. Knowing these situations can help you be proactive and watchful for the signs we just discussed.
The most frequent culprits are gastrointestinal illnesses, often referred to as "stomach bugs," which cause vomiting and diarrhea. Each episode of vomiting or loose stool means a significant loss of fluids and electrolytes. A high fever can also contribute to dehydration because the body loses water through increased sweating and respiration as it tries to cool itself down. Babies who refuse to eat or drink due to a sore throat, mouth sores, or just general malaise during an illness are also at risk, as their fluid intake drops significantly.
Even seemingly minor issues can add up. For example, a baby with a bad cold and nasal congestion might struggle to feed efficiently, leading to reduced fluid intake. Overheating, especially in warm weather or if overdressed, can also cause excessive sweating and lead to dehydration. In all these cases, the body’s fluid balance is disrupted, making it harder for them to stay adequately hydrated without intervention.
When to Call the Doctor Immediately
While this article provides valuable information, it’s absolutely vital to know when to stop reading and pick up the phone to call your pediatrician, or even head to the emergency room. Severe dehydration is a medical emergency, and acting quickly can save your baby’s life.
You should call your doctor or seek urgent medical care immediately if your baby exhibits any of the following: extreme lethargy or unresponsiveness, very dry mouth and skin that "tents" when gently pinched (meaning it stays elevated rather than springing back quickly), no wet diapers for 8 hours or more, significantly sunken eyes and fontanelle, rapid breathing or heart rate, or a complete refusal to drink anything at all. If your baby is under three months old and has any signs of illness, or if vomiting and diarrhea are severe or persist for more than a few hours, always seek immediate medical attention.
Trust your gut feeling. If something feels "off" with your baby and you’re worried, it’s always better to err on the side of caution and consult a medical professional. They have the expertise to accurately assess your baby’s condition and determine the appropriate course of action, whether it’s recommending Pedialyte, intravenous fluids, or other treatments. You are your baby’s best advocate.
Beyond Pedialyte: Holistic Care for a Sick Baby
While Pedialyte can be an important tool for rehydration, it’s just one piece of the puzzle when caring for a sick baby. Holistic care involves much more than just fluid intake. Your baby needs comfort, rest, and continued nutritional support (if possible) to recover fully.
First and foremost, comfort is key. A sick baby often wants to be held, cuddled, and reassured. Keep them in a calm, quiet environment, and ensure they get plenty of rest. Don’t push them to play or engage if they’re not up to it. Managing fever with appropriate medication (as advised by your doctor) and keeping them cool can also make a huge difference in their comfort levels.
Continue to offer small, frequent feedings of breast milk or formula if your baby is tolerating it, even if it’s just sips. These provide crucial nutrients and calories for healing. Once the acute phase of illness passes and rehydration is achieved, gradually reintroduce their regular diet as tolerated. And remember, your unwavering presence and love are the most powerful medicine of all.
Summary & Motivation: You’ve Got This, Parent!
Navigating the waters of baby illness can feel overwhelming, but you’re not alone, and you’re doing an incredible job just by seeking out this information. We’ve covered a lot of ground today, from understanding what Pedialyte is and when it’s appropriate, to spotting those crucial signs of dehydration and knowing when to call for help.
The most important takeaway? Pedialyte can be a valuable ally in the fight against dehydration in babies, but it’s a specialized tool to be used under the careful guidance of your pediatrician. Your baby’s doctor is your best resource for personalized advice, dosage instructions, and ensuring that any intervention is safe and effective for your little one’s unique needs. Never hesitate to reach out to them.
Remember to trust your instincts, stay vigilant for those early warning signs, and prioritize comfort and gentle care for your sick baby. You are their protector, their nurturer, and their first line of defense. Every sip, every cuddle, and every worried call to the doctor shows the immense love you have for your child.
Now it’s your turn! Take a deep breath, use this knowledge to feel more prepared, and know that you are equipped to handle these moments with confidence and compassion. Your dedication and care make all the difference in your baby’s world. You’ve got this, truly!
FAQs: Your Quick Questions Answered
Q1: Can a healthy baby drink Pedialyte for daily hydration?
A: No, a healthy baby does not need Pedialyte for daily hydration. Breast milk or formula provides all the necessary fluids and nutrients for a healthy baby. Pedialyte is an oral rehydration solution specifically designed for rehydrating babies who have experienced fluid loss due to vomiting, diarrhea, or fever. Giving it unnecessarily can disrupt their electrolyte balance.
Q2: What are the side effects of Pedialyte in babies?
A: When used appropriately under medical guidance, Pedialyte generally has few side effects. However, if given incorrectly (e.g., too much, too quickly, or to a baby who doesn’t need it), it can potentially cause electrolyte imbalances, worsen diarrhea (due to sugar content if overused), or cause nausea and vomiting if given too rapidly. Always follow your pediatrician’s instructions precisely.
Q3: How long can a baby drink Pedialyte?
A: Pedialyte is typically used for short-term rehydration, usually for 24-48 hours, or as long as your baby is experiencing significant fluid loss due to illness. It is not meant for prolonged use as a primary fluid source or a nutritional supplement. Your pediatrician will advise you on the specific duration based on your baby’s condition and symptoms.
Q4: Is Pedialyte better than formula or breast milk for a sick baby?
A: No, Pedialyte is not "better" than formula or breast milk. It serves a different purpose. Breast milk and formula are complete nutritional sources crucial for your baby’s growth and development. Pedialyte is a supplemental fluid used for rehydration when a baby is experiencing significant fluid and electrolyte loss. Your pediatrician will guide you on how to balance Pedialyte with continued breast milk or formula feedings, as tolerated, during illness.
Q5: Can I dilute Pedialyte for my baby?
A: No, you should not dilute Pedialyte unless specifically instructed to do so by your pediatrician. Pedialyte is carefully formulated with a precise balance of electrolytes and sugars. Diluting it can alter this balance, making it less effective for rehydration and potentially leading to an imbalance of electrolytes in your baby’s system.
Q6: What if my baby refuses to drink Pedialyte?
A: If your baby refuses Pedialyte, try offering very small amounts frequently (e.g., 1-2 teaspoons every few minutes) using a spoon, syringe, or small cup, rather than a bottle, which might be overwhelming. You can also try offering it chilled. If refusal persists, or if your baby shows signs of worsening dehydration, contact your pediatrician immediately, as they may have other suggestions or recommend a different approach.
Q7: Are there natural or homemade alternatives to Pedialyte for babies?
A: While there are recipes for homemade oral rehydration solutions (ORS) available, it is strongly advised not to use them for babies without explicit instruction and precise guidance from your pediatrician. Getting the balance of salts and sugars exactly right is critical, and an incorrect homemade solution can be ineffective or even dangerous for an infant. For babies, commercially prepared ORS like Pedialyte are generally recommended due to their precise formulation. Always consult your doctor for safe alternatives.